In 2018, I wrote an article for The Mighty titled “Why I Don’t Want to Change my Borderline Personality Disorder.” The piece received a lot of praise from people who felt the same way as I did, but also considerable backlash. I couldn’t understand why there were people hating on the article, until one day, I started to hate it, too.
May is Mental Health Awareness Month — a month aimed at educating about, raising awareness for, and reducing stigma of, mental health and mental illness. While mental health can be managed daily by getting outside, moving your body, staying hydrated, and getting enough sleep, mental illness usually requires medication and therapy and can be a lifelong battle.
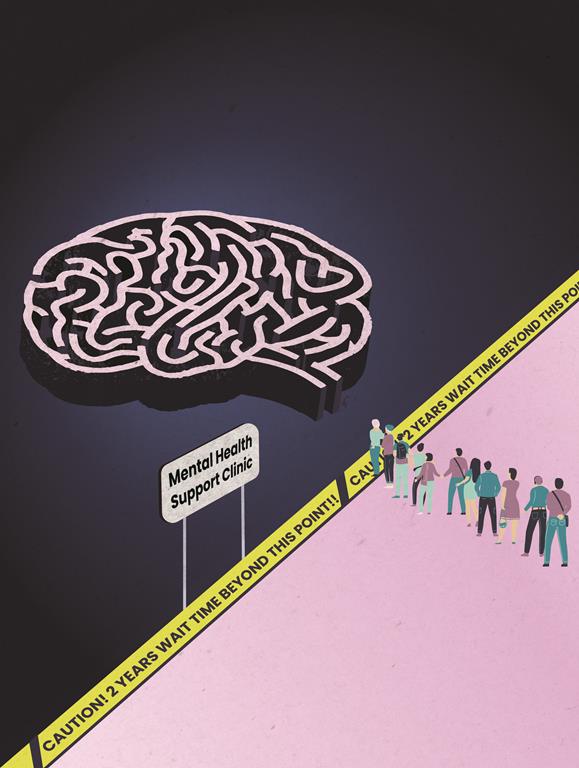
Mental illness is more common than you might think, with one in five Canadians experiencing a mental illness in any given year, and 50 per cent of Canadians experiencing mental illness by age 40. COVID-19 has only made this problem worse; 37 per cent of Canadians experienced a decline in mental health, and the pandemic drastically intensified pre-existing symptoms of mental illness. With such a prevalence of mental illness, shouldn’t there be lots of accessible and effective treatment options?
Treatment is not a one-size-fits-all solution
While there are alternatives, most mental illnesses can be treated with medication, therapy, or a combination of the two. It may sound like a simple solution: just take some pills and talk to a therapist and you should be all better. Unfortunately, that’s not how it works. There are many different medications available, including antidepressants, antipsychotics, stimulants, mood stabilizers, and anti-anxiety medications. Everyone responds to medication differently, and with so many options, it can take years of working with a psychiatrist to find the right drug, combination, and dosages. In addition, because we are facing a shortage of psychiatrists, it can take months or even years just to get an initial appointment with a psychiatrist.
From the time I started taking psychiatric medications, it took roughly five years until I was effectively and stably medicated. I take a combination of four daily prescriptions. I had to try close to a dozen other medications before finding the ones that work for me, and some of the side-effects from those pharmaceuticals made me want to give up entirely. With hundreds of potential options to choose from, meds aren’t a simple solution. However, therapy isn’t straightforward either. There are numerous variations and practices, and they’re staffed by professionals of assorted approaches, and inconsistent abilities.
In my article for The Mighty, I stated that dialectical behaviour therapy (DBT) was not an effective method of therapy. To quote myself directly: “I personally found [DBT] absolutely degrading. Despite it being a life-changing treatment for many people, it created more problems for me than it did solutions.” I truly believed that at the time I wrote the article, and I’m not the only one who didn’t find it helpful, but two years later, I found myself in DBT again, and I realized the problem had been the therapist, not the therapy.
DBT can be extremely effective for treating a number of mental illnesses, not just borderline personality disorder. Like all forms of therapy, it depends on who is providing and receiving it. Aside from DBT, there are a plethora of other options, such as cognitive behavioral therapy (CBT), interpersonal therapy, and psychodynamic therapy. The field is constantly evolving. Practices that were once considered groundbreaking, such as insulin coma therapy and metrazol therapy are now outdated, and new methods such as psychedelic-assisted psychotherapy (which The Cascade reported on last summer), are reemerging. Moreover, new advances in technology allow neuroscientists to analyze the ways our brains function through various neuroimaging techniques, facilitating the development of new medications and treatments.
Therapy can be a lifesaving treatment, but without the right provider it can also be a failure. Many become discouraged because they can’t find the right fit for them, but they may lack access to, or knowledge of other viable options. In my case, I didn’t feel like I had a choice about who my therapists were either time I did DBT, but I lucked out the second time. That is not the case for everyone.
Accessing therapy at all is a battle
If a person has the money, time, and resources to “shop around” for therapists, then that’s great, but for those of us getting their therapy from community mental health centres or who reside in rural areas, the options are often limited.
Why is good therapy so hard to access, though? One reason is that our medical system in general is at a breaking point. Emergency rooms are overflowing, staff are facing burnout, and to top it all off there’s a family doctor shortage. Community mental health centres in B.C. rely on referrals from family doctors, and people in the midst of mental health crises may require emergency room, and sometimes inpatient care. With our healthcare system falling apart in such dramatic fashion, mental health care is falling apart, too.
There’s also a very high demand for therapy right now. While those suffering from severe mental illness are most in need of therapy, people managing their mental health are seeking help, too. And they should, as therapy can be beneficial for almost anyone, but while some people are spending years in therapy for problems that could be solved in a handful of sessions, others spend years searching for support for lifelong psychological ailments. Oftentimes, those with the means to access good therapy on a regular basis have the benefit of financial stability and conscientious employers that support mental health maintenance. Alternatively, those with the greatest need of support for their mental illness frequently suffer from unstable or inflexible employment, limited capital, and provincial health care waitlists.
When I attended therapy through a community mental health centre, I received approximately six months of weekly group DBT, which I found extremely effective. For some, six months is plenty, but many people find it falls short of their needs. While therapy should have a goal, and the goal probably shouldn’t be to stay in therapy forever, it’s important that when people need therapy, they get it. Whether someone needs one session, six months of sessions, six years, or a lifetime, we need to make sure people are getting the assistance they need.
High demand; low (quality) supply
Our increased focus on mental health has produced an influx of self-help books and mindfulness apps. While these tools may be great for managing and emphasizing mental health needs, they do little against severe mental illness, for which meditation and positive affirmations are not a long-term solution.
We need more money funding mental health care (and health care in general), so that we have more doctors, nurses, and therapists, but the way we approach mental health care needs to change, too. Some people aren’t getting treatment at all. Others are getting care that focuses on relieving short-term symptoms rather than looking at long-term treatment. Long-term treatment does exist — we have medications and psychological treatment for basically all mental illnesses — but many aren’t able to access it. These treatments are only effective with comprehensive and continuous care, which most mentally ill people aren’t receiving.
A 2018 report from Statistics Canada shows that 43.8 per cent of Canadians who reported needing mental health care felt that their needs were not fully met. Some are receiving no care, while others are receiving care that is inadequate in amount or quality. With such a high demand for therapists, counsellors, coaches, and other mental health workers, it becomes harder to prioritize hiring people who are great at what they do and easier to settle for low quality supply just to meet the soaring demand.
Nearly half of mentally ill Canadians are going without access to sufficient care — therapy, medication, treatments, and diagnoses. Aside from the obvious implications of not being able to access therapy and medication, there are also serious implications that come from not being able to access a diagnosis.
Diagnoses are an essential tool
When I wrote that article for The Mighty, my diagnosis was, “major depressive disorder, generalized anxiety disorder, and borderline personality traits.” I was only 17 years old, and diagnosing teens with borderline personality disorder is very controversial among psychiatrists. Less than a year later, when I was 18, I was assigned a different psychiatrist, and was given a formal diagnosis.
While psychiatric diagnoses are imperfect, and insufficient on their own (ie. without accompanying treatment), they are also important; they can provide reassurance, decrease feelings of blame, reduce stigma, and help individuals make sense of their mental illness.
For me, my diagnosis helped me escape from the shame that had been pinned on me by comments that made me feel like sharing my thoughts and feelings about my disorder was bad. The negative responses to my article affected me so much that this is my first time writing about mental illness in five years.
My diagnosis has also allowed me to have a thorough understanding of what’s going on in my head; something I wouldn’t have if I didn’t know exactly what my illness was. This understanding allows me to learn how to manage my disorder, gives me the language to speak about what’s happening in my head, and ultimately, makes me feel a whole lot less alone.
Getting through life while mentally ill
While mental illness is the leading cause of disability in Canada, and unemployment rates for severely mentally ill people are as high as 70 to 90 per cent, many of the people disabled from these disorders are not able to access the supports — financial and otherwise — they need because they lack a diagnosis. This leaves a significant number of people, including UFV students, left with no support, no accommodations, and frankly, little to no hope. Canada has made huge strides in recent decades in terms of accessibility and is, as a society, much more understanding and accommodating than the vast majority of countries. That being said, without a diagnosis, that accessibility and those accommodations fall short.
If someone is able to receive a formal diagnosis, this qualifies as a disability, and as such, UFV provides accommodations and accessibility services to students to support their academic journeys. The allowances provided by UFV vary, but given that I typically miss close to half of my in-person classes per semester, these are my accommodations: “This student is eligible for note-taking assistance only for missed classes. If you have a copy of your lecture and/or overhead notes, could you kindly provide it to the student in the case of an absence (if applicable).” Sounds great, right? It’s not that simple.
In theory, it sounds like adequate support, but when you factor in the instructors who don’t have notes on what they talked about in class to email you; don’t provide students with a formal outline or syllabus at the beginning of term; or who place a large grade percentage on in-class activities, things get more complicated. You may opt to drop classes like these early on in the semester and hope you can find better class options, or hope and pray (if you’re into that) that your mental illness won’t render you completely unable to attend classes (at least not this semester).
Accessibility is expanding, but there is still work to be done. COVID-19 exacerbated mental illness, but it also forced our professors to learn how to teach classes — including classes that wouldn’t normally be taught online — via digital platforms like Blackboard and Zoom. Now that we know these classes can be taught online, we should expand that option for anyone who needs it. UFV has a new instructional method called Hyflex, which allows students to complete their coursework either online or in-person, depending on student preference each week. This is a great step, but the courses that currently offer this learning method are limited. Hopefully it will be expanded as we focus more and more on accessibility. UFV also now offers an Accessibility Lab, where all students can go for help with their academic journey.
So, you have your diagnosis and your accommodations through UFV’s accessibility services — now you just have to figure out a way to have enough money to survive. If working isn’t an option because you’re too mentally ill, what are you supposed to do now? The Ministry of Poverty Reduction might be able to help you out… with a grand total of around $1,400 per month, which we all know is hardly enough with rent and grocery prices soaring across B.C.
People with mental illnesses, as with other disabilities, don’t just stop having expenses because they’re unable to work. Mentally ill people still need to put food on the table, keep a roof over their heads, make loan payments, as well as afford utilities, transportation, and tuition. With the amount the Ministry of Poverty Reduction offers, how are they supposed to do any of this when the average monthly rent for a one-bedroom apartment in Abbotsford is $1,500? Many will face the difficult decision to abandon home, friends, and support (the abundance of which comes at a premium) for a more affordable scarcity elsewhere — of healthcare, accommodations, opportunities to learn and work, and social connections. Just because someone is unable to work doesn’t mean they should be unable to live.
The Big Picture
Canada has made huge strides when it comes to how we treat mental illness. One hundred years ago, we were involuntarily sterilizing our mentally ill population. Until 1978, people who were involuntarily hospitalized because of their disorders could have lobotomies performed on them against their will. Things are much better now than they used to be, but we have to keep trying to improve.
While it’s cool that May is Mental Health Awareness Month — we should be aware, always — our work is not done. Our focus and awareness on mental health has created positive change, but those with severe disorders still aren’t getting the treatment (medication, therapy), diagnoses, accommodations, and/or income assistance that they need. While we’re so focused on creating awareness for mental health, do we stop to think about those who are mentally ill?
We need awareness, yes, but we also need faster access to care, higher quality care, better financial support, and more accessibility. Mental illness isn’t going away, so we need to be sure we’re not silencing mentally ill voices in our conversations about mental health. It’s one thing to talk a big talk about mental health awareness but it’s another thing to advocate for those who aren’t mentally healthy.
We must not stay silent when we see injustices that our mentally ill population are facing. We should listen to the needs of our mentally ill population and take action to ensure those needs are met. We need to create space for mentally ill people to live, to work, to play; we need to make sure we aren’t just helping people survive in the short-term, but that we’re creating a world where mentally ill people stay alive in the long-term. We need to stop diluting the issue of mental illness by getting caught up in our newfound passion for mental health. We can’t just talk about mental health, we have to show up for the mentally ill.
Aasha is a BA student, working her way slowly and steadily towards graduating with a major in English concentrating in creative writing and a minor in philosophy. When she’s not busy with her studies, she’s hanging out with her dog, Hendrix, and spending as much time outdoors as possible.